The Value of Artificial Intelligence in Health Care
- Posted by Jim Jordan
- On April 1, 2022
- 0 Comments
The Value of Artificial Intelligence in Health Care
Photo by Gerd Altmann
Today’s digital revolution is full steam ahead, and the extent to which innovations will continue to break barriers is limitless. Artificial Intelligence (AI) best exemplifies how technology has gone beyond expectations. Now, we can experience AI within arm’s reach by simply using our smartphones. From making queries to voice assistants like Siri and Bixby to interacting with rideshare drivers pre-pick up on the Uber app and processing a payment via facial recognition capabilities on one’s iPhone– it is undeniable that there’s an abundance of opportunities for AI advancements for as long as humanity generates and consumes a deluge of data. AI has already started wielding its influence in the healthcare industry, and it will indeed be a crucial element in actualizing our real-time health system (RTHS) aspirations. Before this vision comes to fruition, we must first evaluate what AI genuinely means and how an enterprise-wide definition of the term can potentially yield reasonable business decisions in any organization.
Defining AI
IBM provides two definitions of artificial intelligence. The first one is based on computer science definitions:
“any human-like intelligence exhibited by a computer, robot, or other machines.”
The other definition, on the other hand, is formulated according to how organizations across industries use it:
“the ability of a computer or machine to mimic the capabilities of the human mind—learning from examples and experience, recognizing objects, understanding and responding to language, making decisions, solving problems—and combining these and other capabilities to perform functions a human might perform, such as greeting a hotel guest or driving a car.”
Pretty self-explanatory even for the layman, right? It is essential, however, that our understanding of the concept goes beyond technical and mainstream definitions. Gartner claims that there is no single definition of AI; in fact, enterprises across industries should define AI in their own terms. Let’s take a look at Gartner’s definition:
“AI applies advanced analysis and logic-based techniques, including machine learning, to interpret events, support and automate decisions, and to take actions.”
According to Gartner, two things comparatively led them to adopt this definition: what they perceive as new trends regarding today’s generation of AI technologies and what their clients believe sets it apart from other emerging technologies. Simply put, I think it’s safe to surmise that an enterprise-specific AI definition can reflect a combination of a vendor’s notion of what AI is and does and its customers’ input which may be based on factors like value and purpose. Ultimately, Gartner believes that organizations should be flexible with their definitions. They also suggest that it is essential for business, IT, and data analytics leaders in each organization to come to an agreement as regards the AI definition they should adopt. While they may hold contrasting views, meeting each other half-way and collectively deciding on what AI is to their enterprise as a whole can help them recognize AI-related skills and infrastructure that could best fulfill their company objectives. More importantly, just as I’ve mentioned in my previous blog posts, integrating advanced technologies — in this case, AI — should have a clear purpose. Organizations must be able to acknowledge the relevance of AI in relation to their goals.
Gartner specifically names two general reasons why organizations may consider the need for AI integration:
- AI can employ advanced probabilistic analysis of outcomes to uncover more efficient ways of accomplishing tasks.
- AI can eliminate human-directed steps in the process of task execution as it is already capable of directly interacting with action-responsive systems.
AI may serve a different purpose between enterprises, but what’s important is that you are able to straightforwardly describe why it is a necessary pursuit for your organization.
The following diagram presents the technologies that constitute AI based on the data provided in Frost & Sullivan’s 2018 report on the artificial intelligence market in healthcare:

Oftentimes, non-experts perceive AI and machine learning (which encompasses deep learning) as the same concept, but it’s important that we clearly differentiate these terms from one another.
Machine Learning is essentially a subset of AI; it is the engine that powers most AI advancements. It relies on statistics to discover patterns upon analyzing a vast array of data input (in the form of numbers, words, images, experiences, examples or even clicks), and applies those patterns by making predictions. Most machine learning algorithms use supervised learning whereby systems are trained based on labeled data inputs and expected outputs in order to produce favorable outcomes when facing unfamiliar data.
Photo by Manfred Steger
Deep Learning is a subset of machine learning that uses a multi-layered algorithmic system to process data. Also referred to as hierarchical learning, deep learning organizes data through consecutive layers; each layer “learns” from the output of the previous one to refine outcomes. As data goes through a series of analyses by cascading through each layer, it seems more likely that the processed data would yield accurate connections and representations. Deep learning models are anchored in artificial neural networks (ANNs) which are designed to mimic cognitive learning functions of the human brain. ANNs have comprised of input and output layers as well as a hidden layer whereby input is analyzed to produce meaningful output.

Photo by Ahmed Gad
Natural Language Processing (NLP) is another branch of AI involved in training computers to analyze and manipulate human-generated spoken and written language.
How AI applies in business
To help define what AI means to your organization, delineating the three types of innovations may be a practical first step to take:
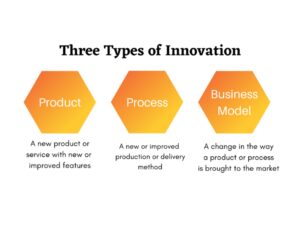
Product innovations are typically visible to the customers and are instigated by factors like technological advancements and a shift in customer preferences. This type of innovation tends to result in a higher demand for the product. On the other hand, process innovations are valued internally as they are invisible to the customer, but often reduce costs. While product and process innovations involve incremental change, the business model innovation type is the riskiest and most challenging since it targets existing frameworks and processes that already strengthen a company’s profitability.
Understanding AI capabilities according to each innovation type can guide organizations in not only discovering the enterprise value of AI systems but also in making decisions that align with their business goals.
AI as a product innovation: Existing AI software and hardware product categories include chatbots, edge AI, conversational user interfaces, smart robots, and quantum computing among other things.
AI as a process innovation: AI supports business processes by promising efficiency and productivity. For instance, predictive maintenance in manufacturing utilizes advanced AI to predict part failures. Another example is how Quality 4.0 uses AI algorithms to manage production quality by digitizing relevant product performance data.
AI creates new business models: Businesses can leverage AI-enabled virtual assistants to schedule appointments and manage events. Meanwhile, AI also enables more sophisticated functions in smart homes such as security and climate control.
How AI applies in healthcare
As cited in an article published by the European Medical Journal, The Harvard Medical Review explains that the innovation process in healthcare can be divided into three categories:
- consumer focus
- technology
- business models
It is interesting to see how these categories somehow parallel the types of innovation discussed in the previous section, though less conspicuously. The difference, however, is that these categories are based specifically on how healthcare innovation should be viewed.
In this healthcare-focused perspective on innovation types, one can assume that a consumer-focused innovation category pretty much speaks for itself. Whether it’s a product or process innovation, the bottom line is it must be adopted for the benefit of patients, payers, clinicians, and other stakeholders. According to the same article, an effective and successful health innovation depends on three factors namely: how patients are seen, how patients are heard, and how their needs are addressed. In short, I think it’s safe to conclude that the success of health innovation is stoked up by simply showing empathy towards patients.
Now, how can healthcare organizations show that they are patient-centric? The rather obvious answer to this question is to make sure that they are able to offer the most convenient and least costly care delivery possible. If health care delivery organizations (HDOs) want optimal care experience for their patients, it appears their best bet would be on technology, specifically in the adoption of emerging technologies.
Taking a step further would mean not only integrating emerging technologies but also understanding the value they bring to one’s business. And if HDOs fully comprehend the worth of big data, they would understand the potential of AI deployment in health care.
In the article “How Artificial Intelligence Helps in Health Care”, Dr. David B. Agus, a professor of medicine and engineering at the University of Southern California, explains that AI in health care pertains to the process in which hospitals and medical practitioners access extensive data sets embedded with what could possibly be life-saving information (e.g. treatment procedures, care delivery speed, and survival rates). Because healthcare organizations have gathered so much data within a span of a decade, leveraging computing power will allow HDOs to utilize that data to improve care delivery. More specifically, computing power can uncover and analyze trends– both large and small– from data sets and predict health outcomes through machine learning.
Machine Learning use cases in healthcare
- Traditional machine learning is utilized in precision medicine, an approach that takes into consideration individual patient variables such as genetics, environment, and lifestyle in selecting the best possible disease treatment procedures. It is clear that HDOs would benefit from this emerging approach to identifying disease and diagnosis as it allows for individualized and targeted care, an outcome that supports one of the goals of RTHS which is to improve the patient care experience.
- HDOs have also started using patient risk detectors which are also based on machine learning models in order to predict heart attacks, strokes, and other life-threatening complications.
- Of the many contributions, machine learning has made to the industry, its impact on cancer research and treatment is perhaps one of the most groundbreaking. Just a few months ago, researchers from Finland successfully developed a machine learning model with the ability to make accurate predictions about how a variety of cancer drug combinations can kill different types of cancer cells.
Deep Learning use cases in healthcare:
- The use of convolutional neural networks (CNNs), a type of deep learning, has been leveraged by care providers, particularly in diagnostic imaging. CNN’s are fundamentally designed for analyzing images, and in the health context, they have provided valuable support in evaluating CT, x-ray, and MRI results.
- Apart from this, CNN algorithms can optimize retinal imaging, specifically in detecting Diabetic Retinopathy (DR) among diabetes patients. In an article published by Medium, 26 layers of CNN algorithms are said to have helped refine retinal image recognition, resulting in equally or even more efficient DR diagnoses compared to that of ophthalmologists.
Natural Language Processing use cases in healthcare:
- In relation to clinical data, NLP can improve the management of unstructured data in an HDO’s electronic health record (EHR) system.
An EHR is the digital version of a patient’s medical history as well as other pertinent data such as lab results, immunization records, and allergy information to name a few. The problem lies in the fact that EHRs are largely unstructured, thus prohibiting the extraction of potentially helpful information. To address this issue, HDOs can turn to NLP. NLP applications have the ability to analyze and organize unstructured data by mining information from doctors’ notes in order to identify synonyms and grammatical patterns, give meaning to the linguistic elements gathered and summarize the information to provide data necessary for achieving optimal care outcomes.
- NLP also enables the real-time conversion of clinicians’ speech into notes through dictation which can be easily accomplished via smartphones.
AI deployment challenges
There is no doubt that the ability of AI systems to process enormous data sets and automate tasks can expand opportunities to enhance care delivery and lower the cost of health care for payers. In addition, adopting AI in healthcare means doctors could spend less time reading and analyzing lab results or medical imagery, hence giving them more time to fully attend to their patients. Although AI can deliver a number of benefits, HDOs must take into consideration certain roadblocks to AI integration. Last year, KPMG released a report that provided fresh insight into the challenges healthcare insiders have been facing when it comes to AI deployment:
- Security and privacy: KPMG reveals that 75% of the healthcare insiders they surveyed are concerned about security and privacy threats that may result from AI adoption, primarily due to the sensitive nature of patient health information (PHI). This seems unsurprising since AI is highly data-driven; its dependence on massive, diverse data sets obliquely permits vendors to collect pools of information from patients. Not to mention, aside from the fact that clinical data cannot be easily altered, there’s so much value in the extractable data medical records carry– from a patient’s medical history to their Social Security Number and banking details– leaving them extra vulnerable to cyber breaches. Other than medical records, attackers can also potentially target other valuable data such as intellectual property in research universities and pharmaceutical companies.
HDOs and their cybersecurity teams should also be wary of “offensive AI”, a cyber offense method employed by attackers which permits them to leverage AI technology, mimicking online user activity in order to hack into a system undetected.
- Cost: 54% of KPMG’s respondents believe that AI has actually increased the overall cost of health care rather than decrease it. The truth of the matter is investing in advanced technologies– whether IoT, edge computing, or cloud-based infrastructure– to boost care delivery outcomes will always be costly. Dealing with AI integration may even more so require a larger budget allocation, and HDOs that are already agonizing over the burden of IT-related expenses may not be able to keep up with it. The skepticism surrounding AI funding is reasonable; however, this further proves the point that HDOs should really pin down what AI means to them and understand how it will achieve both their clinical and business goals. I am hopeful that finding the value of AI will provide HDOs enough motivation to push through with deployment.
- Talent: An important variable measured in KPMG’s report relates to AI training education among medical practitioners and staff, and it’s both worrying but also somewhat expected that only 47% of healthcare insiders surveyed affirmed that their organization provided AI training to its employees. If HDOs were to incorporate AI as a part of their IT ecosystem, part of the investment is providing ample resources and training to all employees. This may even prompt the modification of medical school curricula to accommodate AI training as well as the broader role of digital transformation in healthcare.
Other risks
- Errors: It is important to discern that while AI systems can aid in workflow productivity, they are most definitely far from perfect. This only means committing errors may still be very likely. When AI systems miscalculate data, serious health care repercussions may occur, including putting patients’ lives at risk. Although medical errors already happen even without AI, a slip-up caused by AI systems can be just as, if not more, damaging; once AI becomes more widely used, one faulty AI system can endanger the lives of thousands as opposed to a select number of patients due to one physician’s error.
- Algorithmic bias. AI algorithms cannot be fully trusted unless there’s an abundance of population-specific data on which machines are trained. This can be tricky since historical clinical data is protected, thus restricting access to data that can account for these gaps– especially the ones more representative of certain communities. It has been made evident in medical studies that training data can be biased in terms of race, gender, socio-economic status, and age.
To illustrate this point, a study published in 2019 found that an AI algorithm extensively used in the healthcare industry to determine care management programs shows racial bias against black patients whose opportunities to receive extra care were significantly abridged compared to white patients.
- Lack of supporting infrastructure. With AI, data can be transferred either synchronously or asynchronously, and HDOs don’t quite have the resources to incorporate both systems completely just yet.
Telemedicine best showcases the use of these data transmission methods. For instance, asynchronous telemedicine, also known as “store-and-forward” telehealth, involves temporarily storing data for later transmission (e.g. via email and EHR). To illustrate, physicians can take pictures of their patients’ skin conditions and send them to a dermatologist for evaluation. While seemingly convenient since the patient doesn’t have to visit the dermatologist for an initial in-person consultation, the patient’s wait time for diagnostic results can take longer. On the other hand, synchronous telehealth involves the presence of both patient and care provider usually in the form of live-conferencing. This can be advantageous in emergency situations as well as in providing language translation support to break language barriers in delivering optimal care. Most of all, it saves time and money.
Given these two illustrations, it is easy to see that providing immediate feedback to patients via synchronous care delivery is ideal. But how possible is it to integrate a largely synchronous telehealth system?
Final thoughts
AI is no longer a figment of our imagination. It is here, and it has become more accessible than ever before. While it is obvious that AI can be an essential smart hospital feature because of its ability to enhance patient care experience and business workflows, HDOs must proceed with caution if they’re ever considering full AI deployment on their premises. As mentioned numerous times in previous blog posts, integrating emerging and advanced technologies in health IT ecosystems requires thorough preparation. When it comes to AI, simply jumping on the bandwagon is, frankly, just plain foolish. Instead, HDOs should start by establishing their own definition of AI and understanding why it matters to them. What does it really bring to the table and is it worth the investment? Contemplating on the true value of AI can be useful for HDO and IT leaders in making decisions concerning its implementation. By doing so, they can, for instance, scale their budget to accommodate AI infrastructure and training, among others.
COVID-19 coinciding with the digital transformation age has compelled various industries, especially healthcare, to act boldly. But how bold are we really willing to be to save lives?